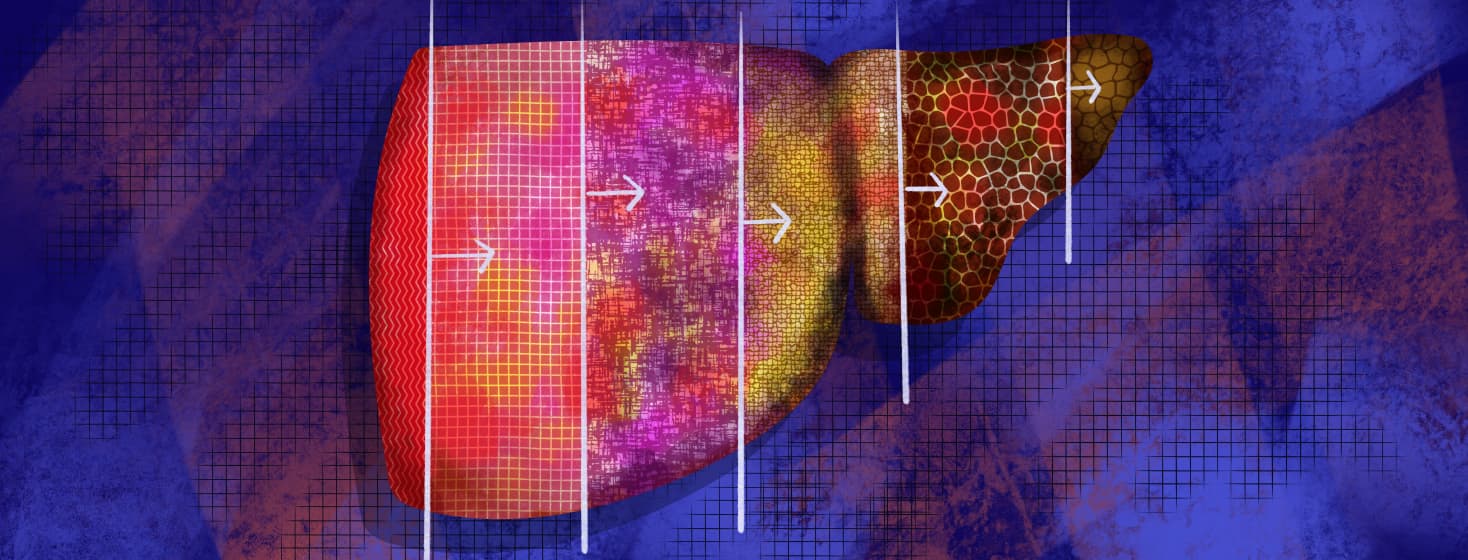
Hepatitis C Phases
Reviewed by: HU Medical Review Board | Last reviewed: February 2022 | Last updated: April 2025
Hepatitis C virus (HCV) can take on different forms or cause different symptoms over time. Some people refer to this as HCV getting worse or progressing.
Some of the common phases of HCV a person with the virus might experience are below.
Acute hepatitis C
Acute (short-term) HCV is the first 6 months of having the virus. But not everyone who is diagnosed with HCV will know when they were exposed. This can make it hard to diagnose someone as having acute HCV. As many as half of all people with acute HCV will fight off the virus without treatment.1,2
Acute HCV may not cause symptoms. If a person does have symptoms, the symptoms usually occur within 8 weeks of the person’s exposure to the virus.
But signs of acute HCV can sometimes take months to appear. Common symptoms of acute HCV include:1,2
- Belly pain
- Nausea or loss of appetite
- Fatigue
- Fever or chills
- Yellowing of the skin or eyes (jaundice)
- Dark urine
- Light-colored stools
- Muscle or joint pain
- Skin itching
Since many people clear the virus on their own, treatment may not be needed if a person truly has acute HCV. There are benefits and risks to treating and not treating during this stage.
Treatment of acute HCV is similar to treatment of chronic HCV.1,2
Chronic hepatitis C
After the first 6 months of HCV, a person develops chronic HCV. Chronic HCV may have few or no symptoms. The virus can continue to reproduce in the liver for decades. Over time, this can cause liver damage.1,3
Some people may not know they have chronic HCV for many years until serious symptoms of liver problems arise. If a person with chronic HCV has symptoms, they may be similar to symptoms of acute HCV.
Other symptoms are general issues, such as:1,3
- Fatigue
- Problems sleeping
- Muscle pain
- Joint pain
Since there are few to no symptoms of chronic HCV, screening tests for those at risk are helpful in diagnosis. Screening tests look for a health issue early and before symptoms occur.
You and your doctor can work together to determine if you are at risk for HCV and if screening would be helpful in your situation. Chronic HCV can be treated with several different types of drugs, including direct-acting antiviral drugs (DAAs).1,3
Fibrosis and cirrhosis of the liver
As mentioned, if chronic HCV is not treated and continues to live and reproduce in the liver, liver damage can occur. The liver has the ability to repair itself.
But there is a limit to how much damage it can recover from.4
Damage to the liver can lead to scarring. Scarring that is reversible is called fibrosis. Permanent scarring is called cirrhosis.
The Metavir scoring system is used to determine how severe liver scarring is. The scale starts at F0 (no scarring), progresses through stages F1, F2, and F3, and goes up to F4 (cirrhosis).4,5
When people refer to HCV getting worse, they are often talking about the progression to fibrosis and cirrhosis. Treating HCV with DAAs can reduce the risk of developing cirrhosis. Cirrhosis can increase the risk of:3,6,7
- Liver cancer
- Fluid buildup (ascites)
- Severe problems with brain functioning (hepatic encephalopathy)
End-stage hepatitis C
Cirrhosis can be split into 2 groups: compensated and decompensated. In compensated cirrhosis, the liver is still functioning relatively well.
Decompensated cirrhosis means the liver is not working well at all or a person has liver failure. Decompensated cirrhosis can lead to serious or life-threatening health issues.7,8
Signs that a person might have end-stage HCV or liver failure are:4,7
- Jaundice that is ongoing or keeps coming back
- Severe itching
- asy bleeding or bruising
- Loss of appetite, nausea, or weight loss
- Swelling in the stomach (ascites) or legs (peripheral edema)
- Trouble breathing
- Confusion
- Trouble with memory or concentration
Bleeding and neurological issues are some of the most severe complications of liver failure. Once a person has liver failure, the only treatment is a liver transplant.
But a liver transplant does not cure HCV. If a person has a liver transplant, they will still need additional treatment to be free of HCV.4,8
Join the conversation