Sponsored: Living Liver Transplants for Hepatitis C
Hepatitis C and its effects on the liver
Hepatitis C is a liver disease caused by the hepatitis C virus (HCV). It is estimated that 3 to 10 million people in the United States are carriers of the virus and a majority are unaware of their HCV status. People are most at risk of getting HCV if they had a blood transfusion or organ transplant before 1992 or were exposed to a needle that had infected blood on it, for example, from a tattoo or piercing.
New HCV treatments offer high cure rates and can clear the body of the virus. For some, even though they have been cured, years of living with the hepatitis C virus may have caused liver damage. Liver damage due to hepatitis C can lead to cirrhosis (scarring) of the liver and liver failure. It is estimated that within 20 years of exposure to HCV, approximately 20 percent of individuals will develop cirrhosis. Another long-term effect of hepatitis C is liver cancer, such as hepatocellular carcinoma (HCC), which affects 20,000 to 25,000 people in the United States each year.
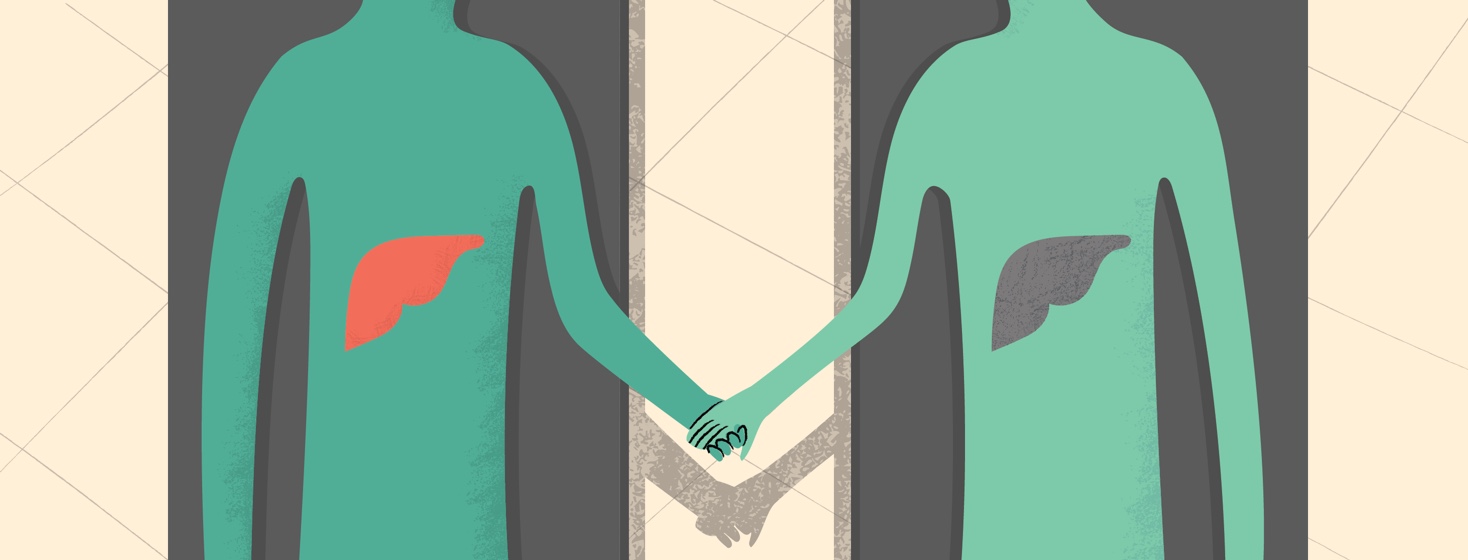
Living-donor liver transplant
Cirrhosis due to chronic hepatitis C is one of the most common reasons for liver transplantation in the United States. A transplant can be immediately life-saving for people with advanced HCV, and can greatly increase the quality of life for someone with chronic HCV, but less advanced disease. However, due to a shortage in deceased organ donation, it can take years before a liver becomes available for transplant.
A living-donor liver transplant eliminates the need for a person to be placed on the transplant waiting list. In a living-donor liver transplant, a portion of the liver from a healthy adult donor is removed and transplanted in the recipient. Donors can be friends, family members, or anyone else who is willing to help. While it is a major surgery for the donor, the majority of them are back to their normal activity and quality of life within a few months after the donation. The donor is able to live a healthy life with the remaining part of their liver, which regenerates within weeks.
Living donors must:
- Be between the ages of 18 and 55
- Be in good physical and mental health
- Have a body mass index (BMI) less than or equal to 32
- Not engage in active ongoing drug or substance abuse
- Have an unselfish desire to contribute to another person’s life in a healthy way
- Be in good general health and have no history of:
- Liver disease, including cirrhosis and hepatitis
- Significant diseases involving the other organs — lung, kidney, and heart
- Pulmonary hypertension
- HIV
- Active malignant cancers
About the University of Pittsburgh Medical Center (UPMC) Transplant Programs
UPMC’s transplant programs are among the world’s largest and are internationally renowned for their influence on the field of transplantation. For more than 30 years, UPMC has provided care to adult and pediatric transplant patients through the Thomas E. Starzl Transplantation Institute, the UPMC Department of Cardiothoracic Surgery, the UPMC Heart and Vascular Institute, and the Children’s Hillman Center for Pediatric Transplantation. Today, UPMC has performed more than 19,500 transplants, including heart, lung, intestinal, kidney, liver, pancreas and multiple-organ transplants, along with heart assist device implantation. A pioneer in the development and refinement of new transplant procedures, UPMC is committed to reducing waiting list deaths through robust living-donor kidney and living-donor liver transplant programs, as well as other innovative methods to expand the donor pool. UPMC also partners with the University of Pittsburgh to advance basic science and clinically applied research, as well as to support the teaching and training of transplant specialists worldwide.
For more information about becoming a living donor and/or liver transplants, please visit http://www.upmc.com/services/transplant or call the UPMC transplant program at 1-877-640-6746.
A note from HepatitisC.net: The content of this article was provided by our sponsor. HepatitisC.net does not specifically endorse or recommend the program, product, medications or therapies discussed in this article.
Join the conversation