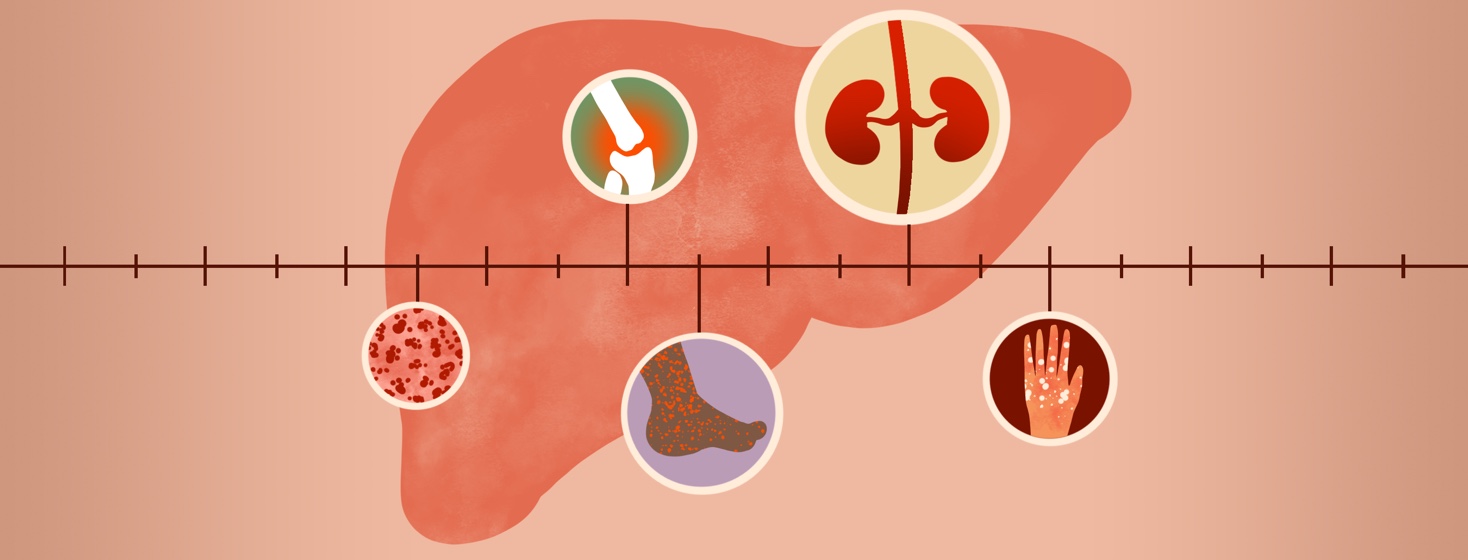
What Are Extrahepatic Manifestations?
Infection with hepatitis C virus (HCV) primarily affects the liver, but other organ systems may be affected as well, especially during chronic HCV infection. When this occurs, these are called extrahepatic manifestations. The most common extrahepatic manifestations fall into 4 main categories: blood diseases, autoimmune disorders, kidney disease, and skin conditions.1 While new treatments for HCV can help reduce the effects of the virus on the kidney and other organ systems, it’s good to be aware of the possible extrahepatic manifestations of HCV so you can get prompt treatment, if necessary.
The four types of extrahepatic manifestations
Blood diseases and autoimmune disorders
These two categories have overlap, which is why they are listed together here.
Multiple studies have found that many people with B-cell non-Hodgkin’s lymphoma (NHL) also have HCV infection.2 HCV is also associated with other diseases like marginal zone NHL and diffuse large B-NHL.2 Doctors believe HCV-related disorders like these occur because of the sustained activation of B cells, environmental factors, genetic factors, and inhibition of B-cell apoptosis (cell death).2
Some people with low-grade B-NHL have responded to antiviral medications to treat their HCV, with increased overall survival.2 For example, Interferon-based treatment and antivirals after remission helped people with slowly-developing HCV-associated NHL live longer and disease-free.2
Joint and muscle pain, also called arthralgia and myalgia, respectively, are other autoimmune manifestations that can occur in HCV infection. Joint pain is reported in 40-80% of patients with HCV infection, and it typically occurs on both sides of the body, mostly in the knees and hands.2 If you develop joint or muscle pain, it’s important to see your doctor to help determine whether this is a result of the HCV infection or a separate rheumatologic disease.
Cryoglobulinemia is the presence of one or more abnormal proteins in the blood that can thicken in colder temperatures. Many people with chronic HCV and cryoglobulinemia have nonspecific symptoms, but Meltzer’s triad is common.3 Meltzer’s triad includes muscle pain, joint pain, and purpura, or purple spots on the skin that are skin hemorrhages. Approximately 30 percent of patients with mixed cryoglobulinemia develop kidney disease.3
Other syndromes that are associated with cryoglobulinemia include peripheral neuropathy, skin ulcers, and lymphoproliferative disorders, as mentioned above with NHL. There are 3 kinds of cryoglobulinemia, and Type II is the most common type seen in those with HCV infection.3 Treatment may consist of antiviral therapy to treat the HCV infection, immunosuppressant drugs, biologic therapies to reduce the number of B-cell clones producing the abnormal proteins, and plasmapheresis.3
Kidney disease
There are several renal, or kidney, diseases associated with HCV infection. The most common HCV-related kidney disease is membranoproliferative glomerulonephritis associated with type II mixed cryoglobulinemia.3 Of patients with cryoglobulinemia, approximately 30% will develop kidney disease.3 To confirm the presence of renal disease, a kidney biopsy is taken. To treat kidney disease in patients with chronic HCV infection, the Kidney Disease Improving Global Outcomes (KDIGO) group recommends treating the HCV infection in those with kidney disease who have no counterindications to the hepatitis C therapy.3
Skin conditions
There are several skin conditions that are associated with HCV infection, including leukocytoclastic vasculitis, porphyria cutanea tarda, and lichen planus.
Leukocytoclastic vasculitis is a small cell vasculitis that can be found in the skin. Symptoms can include ulcers, purpura that are able to be felt, and petechiae (tiny spots due to bleeding under the skin.3 Treatment typically includes HCV therapy.
Porphyria cutanea tarda usually manifests itself as skin fragility, bruising or blistering, hyperpigmentation, depigmentation, and hair growth on the face. This condition is often diagnosed based on clinical symptoms, along with elevated serum, plasma, or urine porphyrin levels. Cornerstones of treatment include staying out of the sun, abstaining from alcohol, discontinuing any iron and/or estrogen supplementation, and regular therapeutic phlebotomy to help restore iron stores and control symptoms. Those who cannot have regular phlebotomy can take an oral iron chelator, but these patients need to be monitored for any retinal damage.3
Lichen planus is caused by a reaction mediated by the immune system that involves CD8-T-lymphocytes and an unknown stimulus. Individuals with lichen planus have approximately a 5-fold higher risk of chronic HCV infection; it is estimated that 10 percent to 25 percent of patients with lichen planus are infected with HCV.3 This skin condition causes flat-topped, purple, itchy lesions on the extremities.
Other areas of the body that can be infected include the GI tract, mouth, genital area, scalp, face, and nails. In most people with the condition, it resolves itself within a year, but others require treatment with a high-potency topical corticosteroid. If the condition is severe or recurrent, oral corticosteroids may be used as a first-line treatment, with other therapies also including systemic retinoids and phototherapy.3
Extrahepatic manifestations: what you should know
There are a variety of extrahepatic manifestations, including some that may not be listed here. If you have HCV, especially chronic HCV, talk with your doctor about the possible other conditions that can arise from the infection. The doctor will be able to provide you with more information about symptoms to look out for, when to call them, and what treatment might entail. It’s also important to remember that even if you have HCV infection, you might not experience any extrahepatic conditions, especially if you got prompt treatment and have an SVR. Each person is different, and your doctor will be able to provide you with information most relevant to your situation.
Join the conversation